KIDNEY TRANSPLANT
1. Purpose
- End-Stage Renal Disease (ESRD): When kidneys can no longer filter waste and excess fluid from the blood effectively.
- Chronic Kidney Disease (CKD): Advanced stages where kidney function is significantly impaired.
2. Donor Sources
- Living Donors: A person who is alive and has agreed to donate one of their kidneys. Living donor kidneys generally have better outcomes due to the kidney’s better condition and the reduced time the organ spends outside the body.
- Deceased Donors: A person who has recently died and whose kidney(s) are suitable for transplantation. The kidneys are preserved until they can be transplanted.
3. Eligibility
- Recipient Criteria: Must have end-stage kidney disease, be otherwise healthy enough to undergo surgery, and have no contraindications to transplantation.
- Donor Criteria: The kidney must be a good match in terms of blood type, tissue type, and other factors to minimize the risk of rejection.
4. Matching Process
- Blood Type Matching: Ensures compatibility between donor and recipient.
- Human Leukocyte Antigen (HLA) Matching: Helps reduce the risk of organ rejection by matching tissue types.
- Crossmatch Testing: Tests for antibodies against the donor’s kidney to prevent rejection.
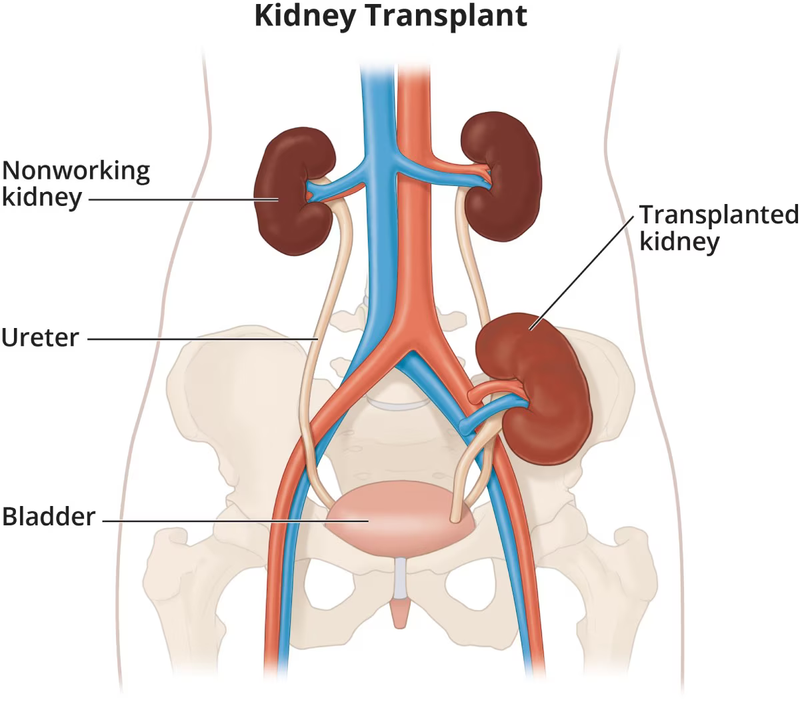
5. Surgical Procedure
- Preparation: Includes pre-surgery assessments, blood tests, imaging, and ensuring the recipient is in good health for surgery.
- Surgery: The donor kidney is implanted into the recipient's abdomen. It is typically placed in the lower abdomen, and blood vessels from the donor kidney are connected to the recipient’s blood vessels.
- Recovery: Post-surgery, the recipient will need to stay in the hospital for monitoring and recovery. Recovery time varies but often includes a hospital stay of 5-10 days.
OPEN KIDNEY TRANSPLANT SCAR

ROBOTIC KIDNEY TRANSPLANT SCAR

6. Post-Transplant Care
- Immunosuppressive Medications: Essential to prevent the recipient’s immune system from rejecting the new kidney. These medications must be taken lifelong.
- Regular Monitoring: Includes frequent blood tests, urine tests, and kidney function assessments to ensure the kidney is functioning properly and to adjust medication dosages.
- Lifestyle Adjustments: Maintaining a healthy diet, avoiding infections, and managing other health conditions are important for the long-term success of the transplant.
7. Potential Risks and Complications
- Rejection: The body’s immune system may recognize the new kidney as foreign and attempt to destroy it. Acute rejection can often be treated with medication if detected early.
- Infection: Due to immunosuppressive therapy, recipients are at a higher risk of infections.
- Medication Side Effects: Immunosuppressive drugs can have side effects, including increased risk of certain cancers and other health issues.
- Surgical Risks: As with any major surgery, there are risks such as bleeding, blood clots, or complications from anesthesia.
8. Long-Term Outlook
- Graft Survival: With proper care and medication, many people enjoy a good quality of life with their transplanted kidney for many years. Long-term survival rates have improved significantly with advances in medical treatments.
- Lifestyle Impact: Most recipients can return to normal activities and work but need to adhere to medical advice and regular check-ups.
A kidney transplant can be a life-saving procedure that improves quality of life and provides a new lease on life for individuals with end-stage kidney disease. For personalized advice and to explore whether a kidney transplant is appropriate, consulting with transplant specialist is essential.


